


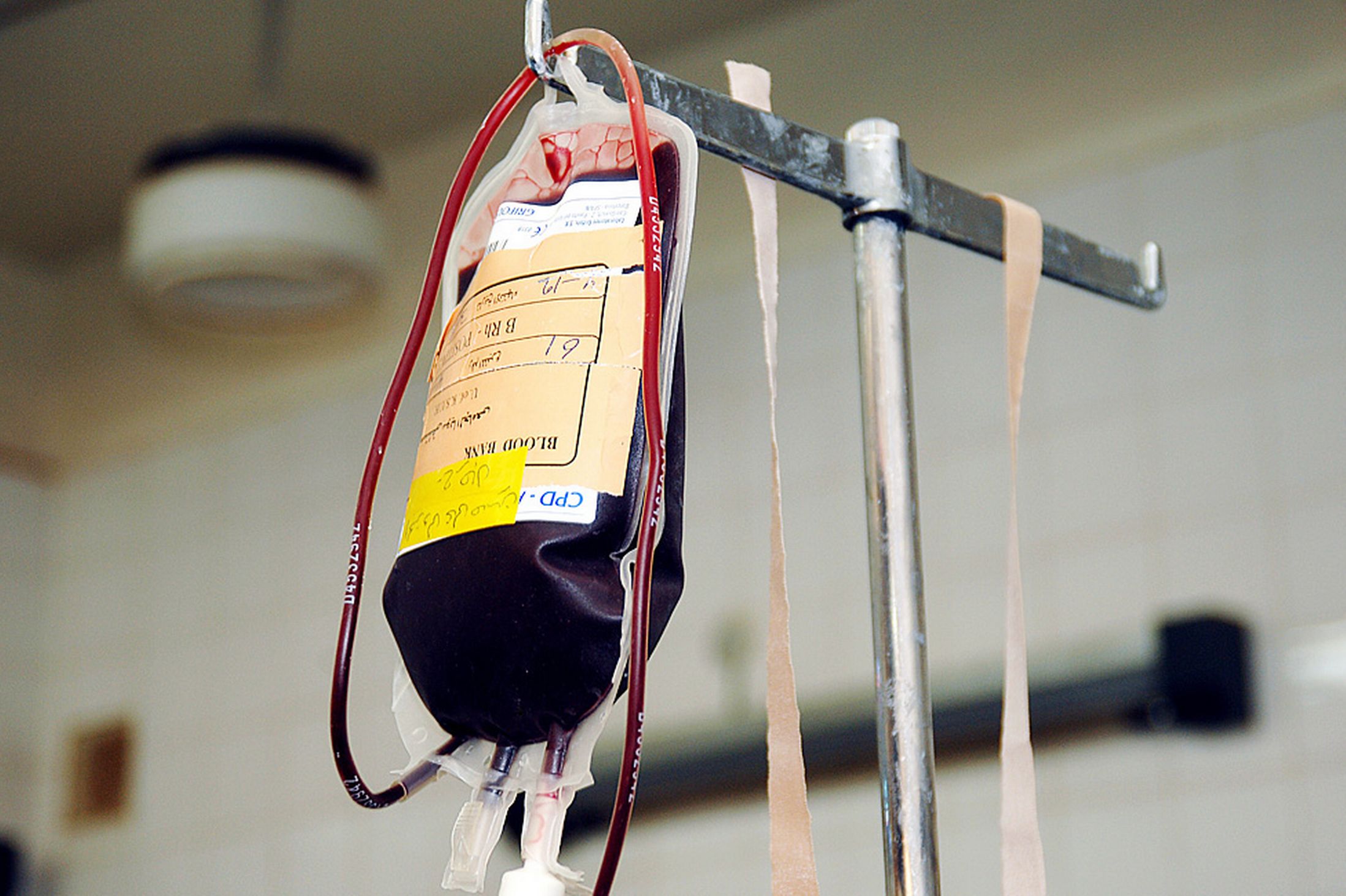
A blood transfusion is a type of medical treatment that involves adding donated blood to your own to replace blood loss, or to supplement some components in the blood that are low. Some patients may also receive some of their own blood, which has been previously extracted before surgery. Blood transfusion is done using an intravenous (IV) line and the procedure usually takes a couple of hours, although it can be done much faster in an emergency.
There are various reasons why you might need a blood transfusion and these include loss of blood due to surgery, injury, or diseases such anemia, cancer, blood disorders, severe liver disease, and more. Anyone who receives blood is at risk for a transfusion reaction, but there are ways to prevent and treat these.
A blood transfusion reaction can occur during or after the process of transfusion. The management of transfusion reactions may vary according to their causes and symptoms.
An allergic or urticarial transfusion reaction to donated blood can occur anytime during a blood transfusion, whether it is your first time or after repeated transfusions. Symptoms of blood transfusion reactions are usually mild and commonly include itchy skin rashes (urticaria), swelling of the arms, hands, legs, and feet (edema), dizziness, and headaches. Less commonly, you may also experience fever, chills, shortness of breath, and swelling of the eyelids or lips.
Causes: An allergic blood transfusion reaction is caused by the reaction of your body’s immune system to foreign proteins/substances in donated blood.
Treatment: For mild symptoms, slowing the rate or temporarily stopping transfusion may be enough. An antihistamine may be administered before resuming the transfusion. Blood transfusion may be discontinued if other symptoms occur and investigation must be done to determine the cause.
This is a serious and potentially life-threatening blood transfusion reaction. Symptoms include shortness of breath, swelling of eyelids or lips, faintness, rashes and clammy skin.
Causes: You can experience this type of reaction if you have anti-IgA antibodies and IgA deficiency.
Treatment: Stop blood transfusion immediately. Administer adrenaline (1:1000 solution) at a dose of 0.01mg/kg subcutaneously, intramuscularly or intravenously. Provide supportive care, which may include airway management if required.
Fluid overload occurs when too much blood is transfused or when the process is done rapidly. It causes your lungs to be filled with excess fluids whereas the heart is not able to pump blood effectively to the rest of the body, resulting in difficulty in breathing.
Older patients and people with heart disease or other serious health conditions are at increased risk of fluid overload.
Cause: Rapid blood transfusion, especially in patients who have cardiopulmonary problems may lead to fluid overload.
Treatment: Stop blood transfusion. Provide oxygen and remove excess fluids using diuretics as required.
Bacterial contamination of stored blood products, particularly platelets, may lead to blood transfusion reactions despite efforts to keep donated blood sterile or germ-free. Symptoms of severe, widespread bacterial contamination (sepsis) from blood transfusion include fever, chills, cold, clammy skin, rapid heartbeat, rapid breathing, confusion, and changes in mental status.
Cause: Bacterial contamination may come from the donor’s skin or equipment used during blood collection and processing.
Treatment: Stop blood transfusion immediately. The hospital blood bank must be notified of the incident. Supportive care must be given and blood cultures taken. Broad-spectrum antibiotics may be started. Sepsis is usually managed by using intravenous antibiotics and aggressive care since this is a life-threatening condition.
Acute lung injury due to blood transfusion is characterized by acute respiratory distress, edema of the lungs, and low blood oxygen levels (hypoxemia), which develop within 2 to 8 hours of transfusion. Diagnosis may be established by chest x-ray, showing lung changes in the absence of heart disease or other possible causes of pulmonary edema.
Causes: Lung changes may be due to the presence of proteins called cytokines in the transfused blood product or may occur due to interaction between your antigens and the donor’s antibodies (or vice versa).
Treatment: Supportive care consists of oxygen administration, which may require tracheal intubation with mechanical ventilation.
You may experience a drop in body temperature while receiving blood transfusion. However, it usually affects infants during exchange transfusion or those undergoing massive blood transfusion.
Cause: Rapid transfusion of large volumes of blood.
Treatment: Use blood warmers during massive blood transfusion or exchange transfusion. Maintain the patient’s body temperature by warming other intravenous fluids and devices.
Citrate is an anticoagulant added to blood products. It binds magnesium and calcium and is metabolized by the liver.Patients at increased risk include those who have liver disease or newborns with immature liver function.
Cause: Rapid transfusion of stored blood in large quantities may cause a drop in calcium and magnesium levels, resulting in depression of heart function and problems in blood clotting.
Treatment: Reduce transfusion rate or temporarily stop blood transfusion to allow citrate to be metabolized. Replacement therapy may be done if you exhibit symptoms of low calcium or magnesium.
A hemolytic transfusion reaction (HTR) occurs when the immune system reacts to donated blood, resulting in the attack of your red blood cells. This reaction may occur immediately or as a delayed reaction days after blood transfusion. Symptoms are similar to other transfusion reactions, including darker urine due to red blood cells destruction.
Cause: Hemolytic reactions are often caused by transfusion of incompatible blood types, which may occur due to human error, such as improper identification of blood samples. Non-immune hemolysis of red blood cells in the container or during transfusion can occur due to other causes, such as mechanical forces, temperature changes, or use of non-isotonic fluid.
Treatment: Stop transfusion immediately. Notify the hospital blood bank immediately. Therapy includes aggressive treatment of low blood pressure and maintenance of kidney blood flow, preferably in the ICU (intensive care unit).
Blood transfusion reactions must be carefully monitored, which, even if uncommon, may be life-threatening. And health care providers must be ready to institute treatment and investigate the cause for the transfusion reactions to protect other patients. Here are a few important things that you should keep in mind:
Blood banks classify donated blood according to A, B, O and Rh types to reduce your risk of transfusion reactions. Before transfusion, your blood and the donor’s blood are cross-matched or tested to see if they are compatible with one another. Then a health care provider checks again to ensure you are receiving the correct blood unit.
There are other alternatives to prevent blood transfusion reactions. You may want to discuss other options with your physician and these include:
Patients who are mentally competent and choose not to accept a blood transfusion have to be treated with sensitivity and respect. Their beliefs, values and cultural background must be acknowledged. These include Jehovah's Witnesses, who often refuse transfusion and are encouraged to detail their wishes about any medical interventions in documents. Should you refuse transfusion of blood or any blood component, you will be asked to sign an appropriate form, which indicates an informed refusal.